Charlie will be 10 on the 9th March 2021 and we are nearly two years on from him falling ill with ADEM in February 2019.
Towards the end of January 2019, Charlie came down with a cold and mild fever. We kept him off school to rest and take medicine to help with the fever, but otherwise he seemed in good spirits and we were even able to take a stroll out in the snow to give his some fresh air.
We weren’t overly concerned to begin with.
However, on the morning of the 6th February, he woke at 4am, told us he felt sick and rushed to the toilet and immediately vomited. He felt hot to the touch and his temperature was over 40. This is a high temperature, but we were used to Charlie having fevers as he had suffered from recurring tonsillitis for six years before they were finally removed in July 2018.
Every bout of tonsillitis had resulted in a high fever so while we were used to seeing those numbers when Charlie had a fever, we were now concerned as this was day nine and he was getting worse rather than better. I called the GP surgery as soon as they opened and they advised to take Charlie up and they would check him over.
The GP asked several times if there had been a break in the fever as sometimes children can lose one virus and pick up another. We knew there had been no break and the GP deliberated for a while before deciding that he would prefer to send Charlie to the John Radcliffe Hospital in Oxford to be checked over.
Because it had been a new GP we had seen that day, I think that may have made a difference with his decision to send us to the hospital as he said he would rather be cautious.
We arrived at the hospital and spent most of the Wednesday in the assessment unit where a chest X-ray and initial blood tests did not cause any cause for concern. However, Charlie’s fever was not fading and he continued to vomit as well as showing signs of fatigue. By 9pm that evening, they decided to keep him in overnight and sent us up to a ward.
By the Thursday evening, Charlie had started to deteriorate rapidly. We had tried to help him to the toilet but he was swaying all over the place, like people do when drunk and we had to hold him up or he would have fell to the floor. We mentioned this to the nurses but they suggested it may have been caused by fatigue from the fevers. But we knew Charlie and how he reacted with a high fever and we had never seen him behave in this way and voiced our concerns with the nurses.
By 11pm, Charlie had started to wet himself which he had not done since a young boy. He could no longer sit upright without falling down and the colour had drained from his face, leaving him a deathly grey colour. Rashes started appearing all over his body but faded as fast as they appeared, only to re-appear somewhere else.
We knew this was not normal for Charlie and pleaded with the nurses to get someone to come and take a look at him. At around 4am on Friday 8th February, a few members of the PICU team came up to take a look at Charlie and as the room filled with more and more doctors, we knew they were listening and something was very wrong. They decided to move Charlie down to the intensive care unit and everything seemed to happen pretty fast after this.
Shortly after arriving in intensive care, the seizures had just started and the team moved quickly to place Charlie on a ventilator and into an induced coma. We were absolutely petrified for him and wondered what had caused him to become so ill.
Charlie was taken for scans. For one of these, we followed his bed along the corridors and were given a fright when the doctors started running with the bed. We were so scared but they remained calm and advised the panic was because he had started to come round and they weren’t ready for him to do that. A lumbar puncture followed to try and find out the cause of his illness.
Finally, just before midnight on Sunday 10th February, the consultant sat us down and told us Charlie had ADEM.
She followed this with the sentence: ‘the boy you knew has gone and you’ve a long, long road of recovery ahead of you.’
I can still hear her say the words in my head and I think we immediately shut down and didn’t fully process the enormity of what was happening. We just went into survival mode and made sure we were there for Charlie.
Sitting next to Charlie’s bed from early morning until late at night made us realise just how incredible the PICU team really were. They constantly spoke to Charlie as if he were awake, telling him every time they touched or moved him and always explaining what they were doing to him, brushing his teeth or filling in a diary entry for him.
We had a particularly bad day where we just sat and watched the numbers on the screen dip and the machines beep, we feared for the worst, but the PICU nurses never showed if they were worried and always offered us reassurance as well as telling us to go eat or take a break.
They were truly incredible – as were our fantastic families who made sure we never had to worry about clothes or food. It just appeared and was one less thing for us to worry about. After about five days in hospital, we were offered a Ronald McDonald House Charity room in the hospital and this was just incredible.
For the whole month we were in hospital, we got to stay in that room and not once did we ever had to feel that feeling of driving away from the hospital knowing our son was still in there. We were always just a phone call and short sprint down the corridors if the worst was to happen in the middle of the night. A place to store our belongings, take a quick shower and a quick snack, even if it was at midnight.
The PICU team made us realise that we had to take care of ourselves too, to be strong enough to be there for Charlie and what may lay ahead. Charlie was started on a course of steroids and had five plasma exchanges over 10 days.
By Saturday 16th, they decided they want to take Charlie off the ventilator. Of course we knew this was a positive step forward but equally we sat nervously waiting while they brought him round. Being able to go in and see him without the ventilator and his eyes open was amazing and when I asked him if he was okay, it was such a massive move forward when he gave the slightest nod of the head, he understood what I had just said! This felt like a miracle.
Intensive care had been such an experience for us. Watching a parent leave ICU without their child is a memory that will stay with us forever and made us even more grateful that our boy was alive and awake. Charlie was moved into high dependency until he had finished the plasma exchanges. At first, there was no movement at all from Charlie’s body and we knew it was a case of wait and see in the beginning.
But slowly, over the next few days, we had slight movement of the fingers on the right side which was a good sign. The physio team moved quickly and gave us some exercises to do on Charlie in the bed as well as having to wear splints as his feet and toes were laying flat in line with his legs. Slowly, he regained some movement back on the right leg as well which were all encouraging signs.
It took over two weeks before we saw any movement coming back on the left hand side of his body. Once the line for Charlie’s plasma exchanges was removed, we were moved up to a general ward to continue his recovery with the Children’s Rehab Team.
In the beginning, Charlie could not talk so the Speech and Language team gave him him a tablet to use which dictated whatever he typed. This meant he could still communicate with us but also gave us some idea that the old Charlie was very much still with us when he regularly typed ‘poo’ and ‘KFC’ into the tablet, hints his personality was still alive even if he was not yet verbal.
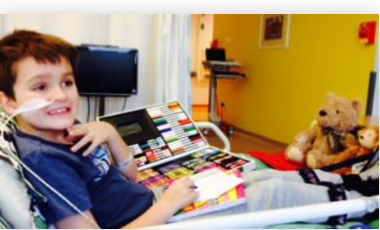
We created a good routine while on the ward and had support from a fantastic rehab team who had the day planned for us, including school, activities with the play team, physio appointments to get Charlie walking again and occupational therapists helping with many tasks like how to fit the wheelchair into the car to hand strengthening exercises with putty.
Charlie was still being fed through a tube, so we also worked with the Speech and Language team to get Charlie eating again, starting with soft food and progressing onto his favourite Cottage Pie! Although it took a while longer to start on fluids and they had to be thickened to start with. They were such a great team and really helped us while in hospital.
It took about three weeks before we finally heard Charlie turn to us late one night and whisper in a faint voice: ‘I’m cold.’ It was very emotional to hear his voice and it was another piece of the puzzle. The steroids had an unexpected affect as Charlie was suddenly constantly hungry. We were not used to this as he had not had much of an appetite before the illness and we found ourselves carrying a bag of grated cheese around the hospital with us for when the urge became to great for him.
Throughout his time in hospita,l Charlie never once complained or cried and got on with everything that was asked of him. We are so incredibly proud of how strong he is. We had been at the hospital for one month when finally at 5pm on the day before his 8th birthday, we were discharged and allowed to go home to continue his recovery.
We arrived home to a room filled with balloons. What an amazing feeling to sit on our sofa with our boy on the night before his birthday in our own home, it was both scary and exciting. The next few months that followed were steroid tablets which caused a large weight gain and a new personality, but this opened him up to new friendships. Where he had once been more reserved, he was now suddenly speaking his mind, although nearly two years on this has faded and he is more reserved once again.
There were also out patient appointments with the hospital physio and occupational therapy teams. We can not thank the Hospital Teams enough, although we did find that sadly, once Charlie was discharged into the Community Teams, there was a lack of support and there are many things we have worked around by finding our own way and what works for Charlie.
We are incredibly grateful that he appears to be recovering so well and thankfully is not requiring much assistance. However, there are many invisible issues that many people do not understand. Yes, it is great that Charlie has recovered so well but people often assume that he is fine now and that’s the end of it.
He is back in full-time school and doing well, although we have also had issues making different teachers understand what he has gone through and how important small breaks are to avoid fatigue, although, even now, we still find at times he is not having them as they feel he didn’t need them or they were too busy.
We find he struggles with his emotions much more and can become teary or angry very quickly although we are finding our own ways to help him. He can also struggle with concentration and at times squirms like he is trying to burst out of his own skin but on the whole he has come so far, at times we wonder how come we were so lucky when we have seen so many other stories where recovery has not been as good.
Apart from the annual check up with the consultant, we are now nearly two years on and have no contact with any teams and this does make us worry for the future if he does have issues pop up from the ADEM, but I guess we will just have to wait and see and for now appreciate where we are.
It was a difficult experience to watch Charlie go through so we can not imagine how families are coping going through this right now with COVID-19 on top. We would also say to any parent to trust your gut instinct. We knew Charlies symptoms were not normal for him and were able to speak up and say so.
He is mostly living the life of your average nearly 10 year-old-boy and if people didn’t know his story, they probably wouldn’t know he had ever been ill. Since falling ill he has gained his green belt in karate, been indoor skydiving and enjoys riding his bike. We truly believe the fact Charlie was already in hospital when he deteriorated and the quick actions of the staff helped him recover so well and we will always be eternally grateful to the incredible NHS for giving us back our wonderful boy in one piece and the boy that we knew is very much still with us.