How the brain works
Last Reviewed 02/10/2023
In order to understand the effects of encephalitis on the brain, it can be helpful to understand how the brain works and interacts with infectious organisms and the immune system. Of course, this is a very complex subject but here we have tried to put together a basic summary to guide you.
The brain
The brain is an amazing organ: it controls everything you think, feel and do. The brain is made up of billions of nerve cells (neurons). A neuron has a cell body containing a nucleus and an axon which carries the impulse away from the cell body. Each neuron makes thousands of connections to other neurons. This ‘neural network’ is similar to the way roads connect to make road networks. In some instances, the axons of neurons are encased in a substance called myelin. This coating acts like the insulation around a wire, making impulses faster and more precise.
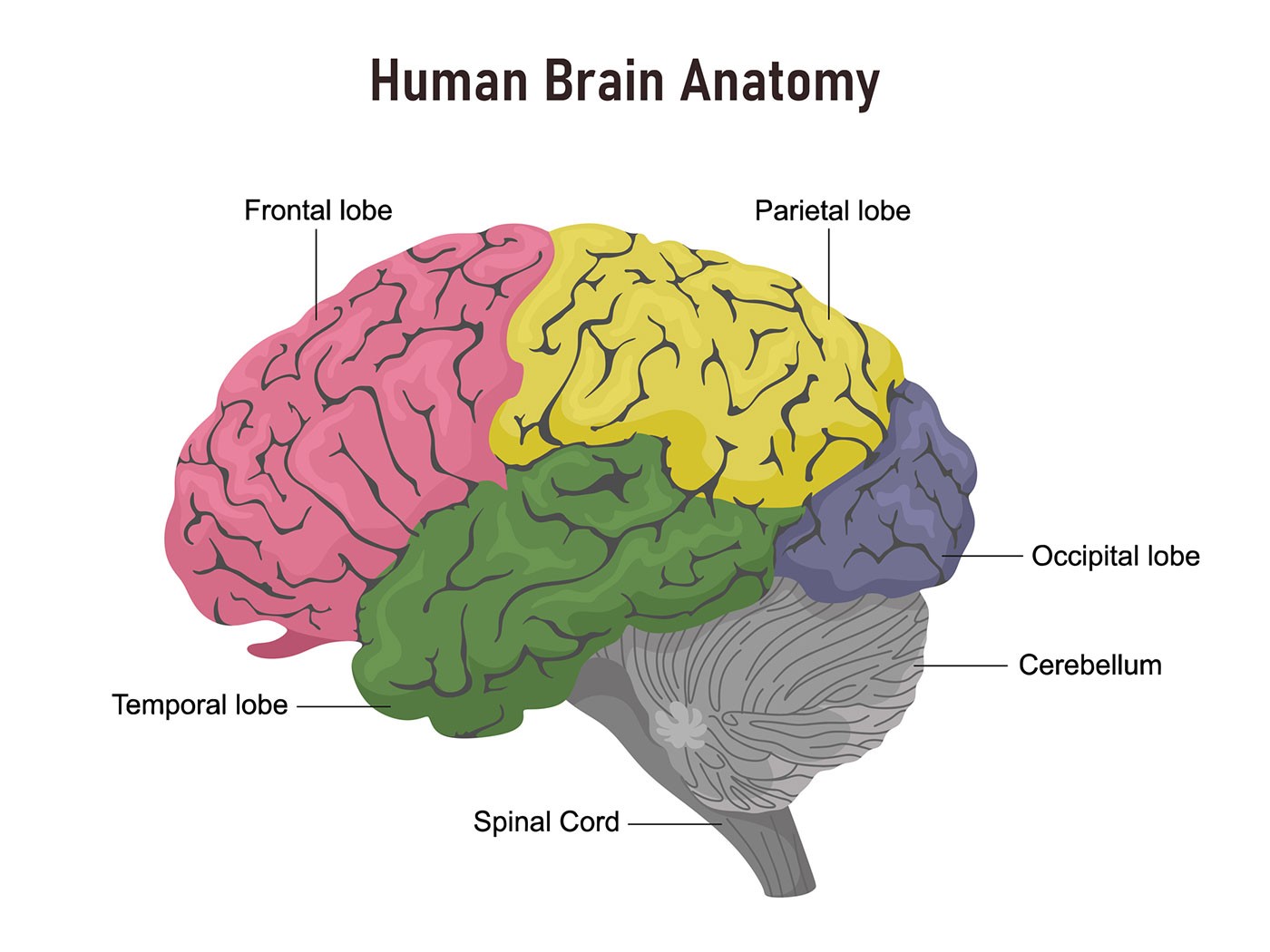
The brain has several areas with different functions and damage to these discrete regions give rise to certain symptoms. These areas of the brain are called lobes. The frontal lobe is involved in decision making, personality and movement. The parietal lobe is responsible for sensation and the occipital lobe for vision. The temporal lobe is responsible for memory and aspects of language. Each of these lobes are made up of the neurons described above and act as the computer processing unit, sending and receiving information from all over the body and interacting with other brain areas.
Quick brain facts:
- The brain uses 20% of the body’s energy.
- The brain has 86 billion neurons.
- The brain’s left and right hemispheres have different functions.
- Quadrillions of synaptic connections exist.
- The brain remains active even at rest.
Image source: John Hopkins Medicine
The brain and infection
The brain is protected by a blood-brain barrier which prevents any large molecules passing from the blood into the brain. The blood-brain barrier acts very effectively to protect the brain from many common infections. Thus, infections of the brain are very rare.
The outcome of any infection is dependent upon the ability of the infection to cause disease and the response of the immune system. The immune response protects organisms against injury and infection by delivering white blood cells to sites of injury to kill potential pathogens and promote tissue repair. However, the powerful inflammatory response also has the capacity to cause damage to normal tissue. Unfortunately the immune response to an infection of the brain can contribute more to the disease process than the infection itself.
The brain and encephalitis
In infectious encephalitis, viruses entering neurons utilise components of the cell in order to replicate (make copies of themselves). This uses up energy stores and oxygen, damaging the cell. In post-infectious / autoimmune encephalitis it is the immune system that causes damage to neurons or other brain cells. In both types of encephalitis, by-products of the immune system’s actions (fluid, white blood cells, the contents of dead nerve cells and disabled viruses) can significantly alter the fluid surrounding neurons and affect their functioning. Cell death causes a fluid build up in the brain. This can cause increased pressure within the skull sometimes causing reduced consciousness
The extra unwanted fluids build up rapidly, and glial cells (cells that support neurons) try to absorb the unwanted chemicals and fluids in order to protect neurons from harm, and in the process they swell up too. Glial cells act as sponges and scavengers of toxic by-products, caused by the inflammation but when they become overloaded, they die and then re-release the toxic chemicals back into the fluid, where they kill additional neurons. The extremely high levels of these substances are sufficient to kill vulnerable and weakened neurons by damaging their membranes or by exciting them to a point where they “burn out” and die.
At the site of inflammation and in nearby tissue, there is biological chaos, as the brain tries to adjust and fight the consequences of the damage. The dying cells give off chemicals that activate macrophages (white blood cells), which move from the bloodstream into the injury area, to absorb and eliminate debris. Glial cells and their helpers, which have gathered at the site to clean it up, now begin to form the scar tissue that will remain a part of the brain’s new architecture. Sometimes, the glial barriers prevent healthy, remaining neurons from restoring axonal connections. In other cases, nerve terminals cannot pass the scar, and abnormal activity is then generated that can lead to epileptic seizures.
Encephalitis and seizures
When a virus enters the brain, their aim is to hijack and replicate healthy brain cells. In both post infectious and autoimmune encephalitis, it is the immune system that causes damage to brain cells.
Regardless of the cause of encephalitis whether it be viral or autoimmune, often the immune system trying to deal with the infection may contribute to the overall inflammation, although well intended.
Epileptic seizures may result in response to the damage resulting from the brain’s inflammation. Scar tissue can develop in the area or nearby the inflammation site, and then interrupt the way neuro-signals are sent around the brain, leading to seizure activity.
Treatment of encephalitis primarily involves managing symptoms and addressing the underlying cause. This can include antiviral medications for viral encephalitis and immune system-modifying therapies for autoimmune encephalitis. Seizures associated with encephalitis can be controlled with antiepileptic drugs.
By Dr Ava Easton, Encephalitis International and reviewed by Dr Mark Ellul, Clinical Infection, Microbiology and Immunology, University of Liverpool, and Dr Ashik Mohamed Babu, Royal Liverpool University Hospital
FS064V5 How the brain works
Page created: August 2002/ Last update: October 2023/ Review date: October 2026
Disclaimer: We try to ensure that the information is easy to understand, accurate and up-to-date as possible. If you would like more information on the source material and references the author used to write this document please contact Encephalitis International. None of the authors of the above document has declared any conflict of interest, which may arise from being named as an author of this document.
Found this helpful?
If you have found this information helpful, please consider making a donation to help us continue our life-saving work in the future. There are many different ways to make a donation, find out more below.
Donate
